Snoring and Sleep Apnea
During sleep, the relaxation of muscles around the airway causes the soft tissues in narrowed areas to vibrate and collide, creating the sound of snoring. As a result of the vacuum effect in the airway walls during breathing, the airway may partially collapse and narrow, leading to reduced airflow—or even a complete obstruction of breathing. When breathing stops for more than 10 seconds, this is called apnea.
To diagnose this, a polysomnography (sleep test) is required. Based on the Apnea-Hypopnea Index (AHI) obtained from this test, sleep-related breathing disorders are categorized into three types:
- Simple snoring
- Upper airway resistance syndrome (UARS)
- Obstructive sleep apnea syndrome (OSAS)
SIMPLE SNORING
If the AHI is below 5, oxygen saturation during sleep is above 90%, and the pressure in the esophagus during inhalation does not fall below -10 cm H₂O, the condition is considered simple snoring.
SIMPLE SNORING
- An AHI of 5–20 indicates mild apnea,
- 20–40 indicates moderate,
- Above 40 indicates severe apnea.
WHO IS AFFECTED?
What’s often assumed to be just snoring can actually be a mild form of sleep apnea. Among men under 30, the prevalence is around 30%, and this rises to 60% in men over 60. There is a direct correlation between body weight and snoring. Overweight individuals are more likely to experience both snoring and sleep apnea.
Mild sleep apnea is more common, while moderate and severe cases are less frequently seen. Moderate obstructive sleep apnea is observed in approximately 2% of adult men, while severe apnea is seen in only 0.3% of men aged 35–60.
TREATMENT OF SNORING AND SLEEP APNEA
Treatment varies depending on the severity of the condition and the location of the airway obstruction. Non-surgical options include:
- Lifestyle modifications
- Medication
- Pressurized air masks (CPAP)
- Oral appliances
LIFESTYLE CHANGES
Most people with snoring or sleep apnea are overweight. Excess weight contributes to sleep apnea, and sleep apnea, in turn, lowers oxygen intake and slows metabolism, increasing fatigue and leading to further weight gain. Therefore, achieving ideal body weight is a key goal.
Smoking, sedatives, and alcohol worsen sleep apnea and should be avoided.
Sleeping on the back is not recommended. Side-sleeping is the ideal position.
If nasal congestion is present, the underlying cause should be diagnosed and treated.
Other underlying medical conditions, such as hypothyroidism, should be identified and managed, as they can contribute to sleep apnea.
POSITIVE AIRWAY PRESSURE DEVICES (CPAP)
The CPAP (Continuous Positive Airway Pressure) device is one of the most effective non-surgical treatments for sleep apnea. It works by providing continuous air pressure to keep the airway open during sleep, counteracting the collapse caused by negative pressure.
CPAP is suitable for:
- Patients who refuse or are not eligible for surgery
- Patients who do not benefit adequately from surgery
- Pre-surgical preparation
ORAL APPLIANCES
There are two main types of oral appliances:
- Devices that pull the tongue forward
- Devices that advance the lower jaw
More than 75% of simple snorers see improvement with these devices. However, side effects such as increased saliva or dry mouth are common. Long-term use may lead to jaw joint issues.
SURGICAL TREATMENT OF SNORING AND SLEEP APNEA
Surgery is planned according to the underlying cause. For example:
- If nasal obstruction is the cause, septoplasty or turbinate reduction may be necessary.
- If enlarged tonsils or a long uvula contribute to the problem, surgery may target these areas.
- Additional options include operations involving the soft palate, tongue base, or even the jaw.
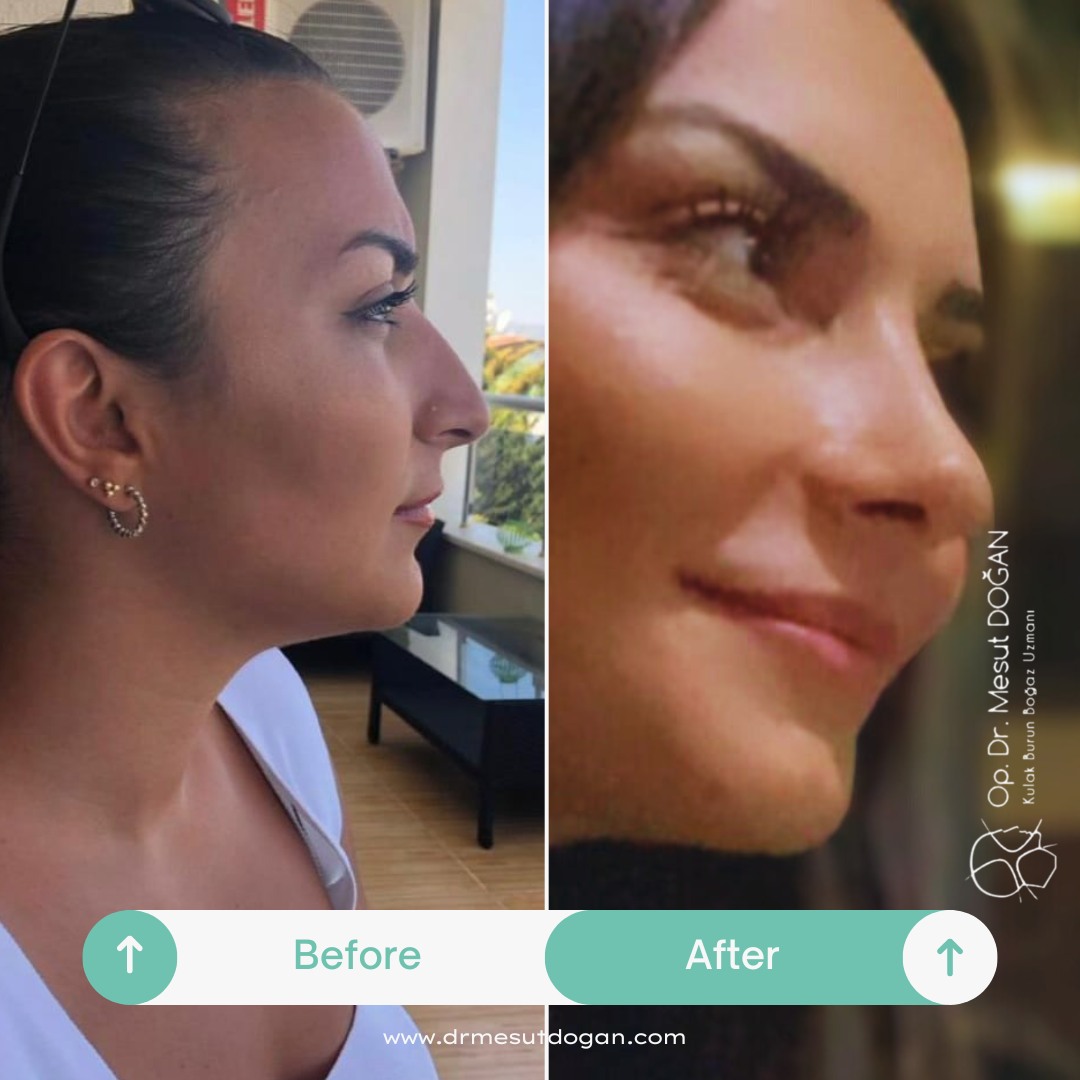
Patient Reviews
I chose Dr. Mesut Doğan for my rhinoplasty operation, and I’m incredibly satisfied with the result. I now have a nose that looks natural and suits my face perfectly. He was attentive throughout the entire process, both before and after the surgery. I’m so glad I chose him!

I had been unhappy with my nose for years but kept postponing surgery out of fear. Thanks to Dr. Mesut Doğan, I was able to overcome all my fears. A natural appearance and being able to breathe comfortably were very important to me — and he delivered both. I’m truly grateful to him and his team.

I did extensive research on rhinoplasty and decided that Dr. Mesut Doğan was the right choice. From the very first consultation, he and his team made me feel confident and reassured. After the surgery, I achieved an excellent result both aesthetically and functionally. I’m so glad I met you, doctor!

I consulted Dr. Mesut Doğan for rhinoplasty and the result exceeded all my expectations. My nose looks so natural that no one can even tell I had surgery. He was by my side with his warm attitude and professionalism at every stage of the process. Endless thanks!

I had been unhappy with both the appearance of my nose and breathing problems for a long time. After meeting Dr. Mesut Doğan, I knew I had made the right decision. My surgery went very smoothly, and I’m extremely happy with the way I look now. I wholeheartedly recommend him to everyone.

Frequently Asked Questions
Most Frequently Asked Questions About Rhinoplasty
How Long Does a Rhinoplasty Surgery Take?
On average, it takes about 2 to 2.5 hours. The duration may vary depending on the specific procedures performed.
When Can I Take a Shower After Nose Surgery?
You can take a shower during the first 2 weeks as long as you avoid getting your face wet. You can wash your hair by tilting your head back and wash your body carefully without letting water touch your face. After 2 weeks, there are no restrictions.
Can I Get My Face Wet After Nose Surgery?
You should avoid getting your face wet for the first 2 weeks.
When Will My Nose Fully Settle After Surgery?
It usually takes between 6 months to 1 year for the nose to fully settle into its final shape.
Will There Be a Scar After Rhinoplasty?
There may be a very faint and barely noticeable scar under the nose.
Do I Need to Follow a Diet After Rhinoplasty? Are There Any Forbidden Foods?
There is no need for a special diet, and there are no food restrictions after surgery.
When Can I Return to Work After Nose Surgery?
Most patients can return to their daily routines the very next day. They can go out and manage their daily tasks comfortably. However, we recommend resting — not necessarily in bed — for the first week. Returning to work is generally suitable after the nasal splint and packing are removed, about one week post-surgery.
What Type of Anesthesia Is Used During Rhinoplasty?
Rhinoplasty is performed under general anesthesia.
When Are the Nasal Tampons Removed?
They are removed one week after the surgery.
When Is the Splint Removed?
The splint is also removed one week after the surgery, together with the tampons.
When Are the Tapes Removed?
At the one-week check-up, when the splint and tampons are removed, the tapes are replaced with new ones. The tapes are usually kept for another week, so in total, tapes remain in place for 2 weeks.
Will I Experience a Lot of Pain After Rhinoplasty?
No. Any discomfort can be easily managed with mild painkillers.
Can I Wear Makeup After Nose Surgery?
Yes, after 2 weeks. Makeup is allowed along with showering.
Are There Massage Techniques to Reduce Swelling?
Gentle downward massages from the bridge of the nose can help reduce swelling. However, since patients tend to apply too much pressure, we usually don’t recommend it strongly.
Is There Any Medication That Helps Speed Up Healing?
There are special creams available for bruising. Your doctor will recommend one after the surgery.
What Are the Advantages of the Piezo Technique?
Piezo surgery targets only the bone tissue without damaging the surrounding soft tissues. Since it doesn’t harm soft tissue, under-eye bruising and swelling are minimal. The recovery process is faster, and it provides greater ease during the surgery.
When Does Under-Eye Swelling Go Away After Nose Surgery?
Thanks to the Piezo technique, swelling is minimal and typically resolves within 2–3 days.
When Does Under-Eye Bruising Go Away After Nose Surgery?
Again, due to the Piezo technique, bruising is minimal and usually disappears after about one week.
Will My Nasal Congestion Be Treated During Rhinoplasty?
Yes. Addressing breathing problems such as nasal congestion is one of the core principles of rhinoplasty.
Can the Nose Drop After Surgery? What Causes It?
Yes, if the structural support of the nose is compromised, it may drop. That’s why the surgical technique and the attention and skill of the medical team are extremely important.
Can Anyone Have a Nose Surgery?
Rhinoplasty is not recommended for individuals under 18, as their nasal development is not yet complete. It also cannot be performed on patients with certain health conditions that make general anesthesia risky.
Is There an Age Limit for Rhinoplasty?
Since nasal development is usually completed by age 18, we do not recommend surgery for anyone younger.
Can Both Cosmetic Correction and Deviated Septum Be Fixed in One Surgery?
Absolutely. Both procedures can be done in a single session.
Will I Need Someone to Take Care of Me After Surgery?
No, you’ll be able to manage your daily activities on your own. However, it’s beneficial to have someone accompany you during your overnight stay at the hospital.